And does it know when to stop tunneling?
![]()
This is disappointing:
But as someone with Crohn’s (for almost 60 years), I figure it’s still a good idea. I estimate I’ve had about 25-30 of them over my life. No big deal, as long as anesthesia is used.
But the prep . . . . ![]()
There are significant issues with this particular study. Probably the biggest one was that they counted people who were invited to get the 'scope but didn’t actually do it, which was a majority of the participants.
The philosophy of colonoscopies is somewhat different here in Europe than it is in the US.
A good layman’s-level analysis: Colonoscopy: What to know after study questions its effectiveness | CNN
A more technical study done in the US that shows considerably different results: https://www.nejm.org/doi/full/10.1056/nejmoa1301969
That’s a relief. I find this appalling though:
Dominitz says one reason might be that most people in the European study didn’t have sedation when they got their colonoscopies. Only 23% of the patients in the European study received sedation, but virtually everyone having a colonoscopy in the US gets it. Colonoscopies can be uncomfortable, and doctors might, without even realizing it, be less thorough if people are in pain.
Does the lack of anesthesia include children? My experience with exactly that, was, to me, a form of sexual abuse, despite it being of the best intentions (I hope).
Part of that “philosophical” thing I mentioned is that many of what European medicine calls “colonscopy” would be better called “high sigmoidoscopy.” here. Unless there’s a reason, most European screening colonoscopies do not include the ascending colon, only the sigmoid and left part of the descending colon where polyps and cancers are most common. Yes, they are commonly performed as outpatient clinic procedures without anesthesia. As far as I know, screening colonoscopies are never performed on children, only adults beginning at middle age.
Traditional US-style colonoscopy tends not to be used for screening at all here; we have several chemical and DNA-based lab tests performed on stool that have not yet become popular there. Part of that is that your FDA tends to be very conservative about authorizing DNA testing for this purpose.
The lab I worked at in the US tried several times to make DNA stool testing into a thing, mostly unsuccessfully. Routine iFOBT and FIT-DNA tests detect cancers and growing polyps pretty well. As far as I know, the only one currently approved in the US is Exact Science’s Cologard. Part of that is due to an earlier test, Pregen Plus, being rushed to market before it was completely ready, 20 or so years ago.
Alas, I know little about Crohn’s from a diagnostic perspective, despite both my mother and my sister being diagnosed with it and having iliostomies done as adults. That was some time ago, before the biological treatments that are now available existed.
I agree, screening tests wouldn’t be done on kids, but if disease is suspected, it is one of the few ways that internal organs can be examined non-invasively (i.e., without surgery). I assume kids with suspected colitis would get examined that way, but I’m not an expert. There is a test that can detect Crohn’s disease from stool, but if found further tests have to be done to determine where in the GI tract, the extent, and so on.
I’m sorry to hear your family has had to have surgery and ostomies. I’m lucky to have avoided them so far.
I had a lower GI (barium enema xrays) done once and there was no anesthesia or sedation. It was a bit weird and unpleasant, but not really painful. I know that’s different from a colonoscopy, but I don’t know how different. Knowing that they use sedatives or anesthesia for it makes it seem a little more scary.
I think anesthesia is used for a colonoscopy because colon cancer often starts with a polyp that has a lesion at the end, and the physician can immediately remove it with the 'scope. It’s one of the few situations where suspected cancer of an internal organ can be detected and removed at the same time. That can be painful, so the anesthesia is warranted. At least, I think it could be; I’ve had aches for a few days afterward when one is removed (non-cancerous so far, but it’s not good to just leave them).
I haven’t had a barium x-ray in decades, but my experience was the same as yours – no anesthesia. It’s worse when it’s an air contrast study, where air is pumped in after introducing the barium. A thin layer of barium is formed between the lining of the colon and the air, which outlines the lining for better examination. The last time I had one of those, the idiot radiologist forgot to put the air in, making the procedure a waste of time, money, pain, and stress. Or the idiot gastroenterologist forgot to order it. In a follow up appointment, the GI doc said, “oh well, you’ve had colitis so long we need to take your colon out”–without any up-to-date data. Fortunately I said “fuck that” (not out loud, alas) and still have all my plumbing today.
The simulation video is fascinating:
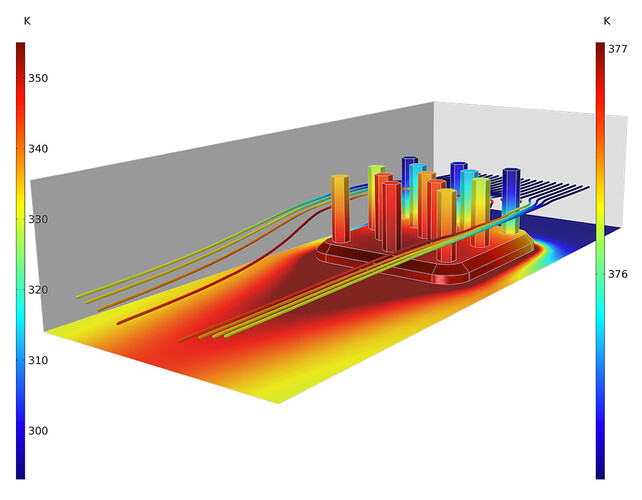
I’d like to see one colored by temperature. Maybe it is, but if so it’s only using a yellow to red spectrum. They should use a color patterns that has a wider range like this:
But that edge comes at a cost: It increases a person’s risk of autoimmune diseases. “The exact same genetic variant that we find to be protective against Yersinia pestis is associated with an increased risk for Crohn’s disease today,” Barreiro says.
When evolution gives, it also takes away.
At first I thought it was carrying a tea towel. “May I take your order, ma’am?”